The Alarming Link Between Viruses and Cardiovascular Health
Viral infections increase heart attack risk, according to new research that sheds light on how common illnesses may affect long-term heart health. For decades, medical science has recognized that infections can have far-reaching consequences beyond their immediate symptoms. However, recent studies have revealed a troubling connection between viral infections and cardiovascular disease. A comprehensive meta-analysis published in the Journal of the American Heart Association has confirmed that common viral illnesses such as influenza, COVID-19, HIV, hepatitis C, and shingles can heighten the risk of heart attacks, strokes, and other serious cardiovascular complications.
The research analyzed 155 studies spanning several decades, using global data to explore how viruses influence the cardiovascular system in both the short and long term. According to the findings, individuals who contract the flu are up to six times more likely to experience a heart attack within the month following infection. Similarly, those who have suffered from COVID-19 face nearly double the risk of developing cardiovascular complications compared to those who have not been infected.
Lead author Dr. Kosuke Kawai, adjunct professor at the David Geffen School of Medicine at UCLA, emphasized that vaccination offers a dual advantage — not only preventing infection but potentially safeguarding heart health as well. “Often, we get vaccinated to reduce the risk of influenza or other illnesses, but vaccines can provide an additional benefit in terms of protecting against cardiovascular disease,” he noted.
The Science Behind Viral Infections and Heart Disease
The association between viral infections and heart disease is complex but biologically plausible. When a virus enters the body, the immune system activates an inflammatory response to fight off the infection. In some cases, this inflammation becomes excessive, causing collateral damage to the blood vessels and heart tissue.
Dr. Scott Roberts, associate medical director for infection prevention at the Yale School of Medicine, explained that respiratory viruses increase cardiovascular risk in two main ways. The first is indirect, through inflammation that leads to stress on the cardiovascular system, blood clot formation, and the disruption of normal blood flow. The second is direct, where certain viruses can infect the heart muscle itself, causing myocarditis or other forms of heart tissue injury.
“Unfortunately, many infections can do this,” Dr. Roberts said. “Generally, the more severe the viral illness, the greater the risk of cardiovascular complications.”
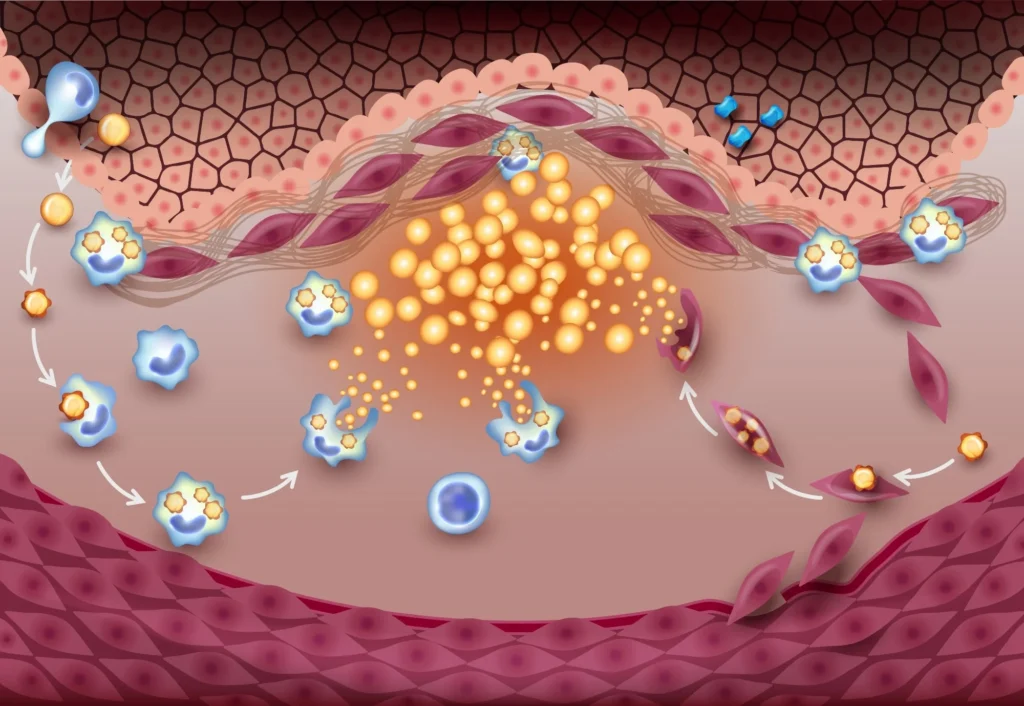
Inflammation plays a central role in this relationship. Cytokine storms—excessive immune responses triggered during severe infections—can cause damage to arteries, making them more prone to plaque rupture, a leading cause of heart attacks and strokes. Moreover, persistent inflammation can lead to long-term scarring and stiffening of heart tissues, which impairs cardiovascular function even after recovery.
Short-Term and Long-Term Effects
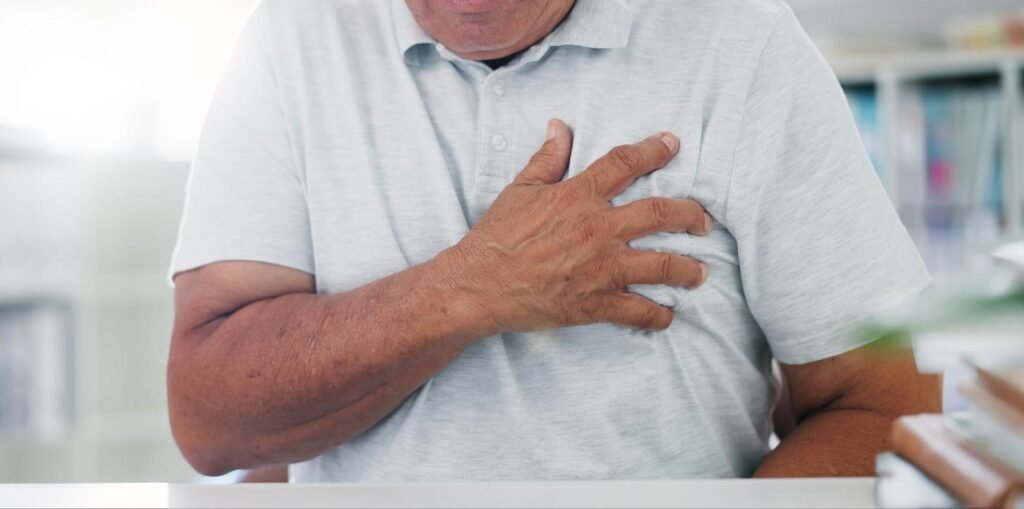
The study’s findings show that the risk of heart attacks and strokes is especially high in the immediate aftermath of infection. Within weeks of contracting the flu or COVID-19, patients are more likely to experience cardiovascular events due to elevated inflammation and blood clotting activity. However, chronic viral infections—such as HIV, hepatitis C, and shingles—carry a different kind of danger: they can increase cardiovascular risk over the long term.
These viruses often persist in the body for years, keeping the immune system in a constant state of activation. This prolonged inflammation gradually damages blood vessels and accelerates the development of atherosclerosis, a condition where fatty deposits build up inside arteries. Over time, this process can lead to coronary artery disease, stroke, and heart failure.
Dr. Kawai noted that while acute viral infections pose immediate risks, chronic infections act more subtly, often causing years of silent damage before symptoms of cardiovascular disease become apparent. “It’s not just the patients who have underlying increased risk for cardiovascular disease that might be at greater risk,” he said. “Those who are younger adults, or people who might not necessarily have traditional risk factors, are also vulnerable after a viral infection.”
Understanding the Mechanisms of Damage
When viruses trigger inflammation, the immune system releases various proteins, including C-reactive protein (CRP), interleukin-6, and tumor necrosis factor-alpha. These compounds are known to damage the endothelium—the inner lining of blood vessels—making it easier for cholesterol and other substances to accumulate.
In the case of COVID-19, researchers discovered that the virus can directly attack the ACE2 receptors in heart and lung tissues, leading to inflammation, microclot formation, and oxygen deprivation. This mechanism helps explain why patients recovering from COVID-19 often experience lingering symptoms such as chest pain, shortness of breath, and fatigue—collectively known as “long COVID.”
Similarly, influenza viruses have been shown to destabilize arterial plaques, while shingles (caused by the reactivation of the varicella-zoster virus) can inflame blood vessels and increase stroke risk, particularly in older adults.
Even less common infections such as cytomegalovirus, herpes simplex, and human papillomavirus (HPV) have been linked to cardiovascular complications, though further studies are needed to establish the exact biological mechanisms.
Prevention Through Vaccination
The evidence is increasingly clear that vaccination plays a crucial role in reducing cardiovascular risks associated with viral infections. Immunization helps prevent severe illness, reducing the chances of inflammatory responses that can damage the heart.
Dr. Roberts explained that vaccines work by presenting the immune system with a harmless version of the virus or its components. This controlled exposure allows the body to build immunity without triggering the harmful inflammatory cascade seen in actual infections. “Vaccines for many of these viruses exist and generally lessen the risk of cardiovascular events after infection,” he said.
Flu shots, COVID-19 vaccines, and shingles vaccines have all been proven to reduce not only infection rates but also the severity of illness, which translates to fewer cardiovascular complications. Health authorities continue to encourage adults, especially those with preexisting conditions like hypertension or diabetes, to stay up to date with recommended vaccinations.
The Broader Public Health Perspective
Cardiovascular disease remains the world’s leading cause of death, responsible for nearly 18 million fatalities each year. The new findings suggest that managing viral infections is a critical component of reducing this burden.
Public health officials are urging integrated preventive measures—combining vaccination, antiviral treatments, and lifestyle changes—to address the growing evidence linking viral infections to heart disease.
Dr. Kawai and his co-authors concluded, “Our study highlights the importance of preventive strategies, especially for adults with traditional cardiovascular risk factors. Vaccines may play an important role in mitigating the risk of cardiovascular disease.”
As populations age and new viral threats emerge, health experts emphasize the need for global collaboration to monitor, prevent, and manage viral-induced cardiovascular complications.
The Global Perspective on Viral Infections and Heart Disease
While the connection between viral infections and heart disease has long been suspected, this new analysis reinforces just how global the issue has become. According to the World Health Organization (WHO), cardiovascular disease remains the leading cause of death worldwide, accounting for approximately one in every three deaths. The growing evidence that viral infections can act as a hidden catalyst adds another layer of urgency to the global fight against heart disease.
Health authorities from multiple countries are now reevaluating how vaccination campaigns, infection control policies, and public health education can collectively reduce cardiovascular risk. The WHO has acknowledged that viruses such as influenza, SARS-CoV-2 (the virus that causes COVID-19), and herpes zoster can directly or indirectly contribute to cardiovascular complications.
In a statement regarding viral and chronic disease links, WHO health experts have highlighted that infection prevention through vaccines could significantly reduce cardiovascular disease burden globally. Countries with high vaccination rates for influenza and COVID-19 have already reported lower instances of post-viral cardiac complications. https://www.health.harvard.edu/heart-health/flu-and-heart-attack-risk
Viral Infections and Long-Term Heart Damage
The effects of viral infections on the heart are not always immediate. In some individuals, the damage may unfold silently over years. Chronic viral infections, such as hepatitis C and HIV, can persist in the body for decades, leading to sustained inflammation and vascular injury. Research has shown that even after viral clearance, the residual inflammation can continue to pose cardiovascular risks.
A recent analysis from researchers in the United Kingdom found that individuals with a past history of viral infections exhibited higher coronary artery calcium scores, suggesting accelerated plaque buildup. This supports the hypothesis that viral infections can play a role in the early stages of atherosclerosis.
The mechanism behind this is multifaceted. Persistent Viral infections increase heart attack risk particles or proteins can remain in tissues long after recovery, causing the immune system to remain slightly activated. This low-level inflammation increases oxidative stress, damages endothelial cells, and leads to arterial stiffness — a known precursor of heart disease.
The Hidden Impact on Younger Populations
One of the most surprising findings in the new meta-analysis was that younger adults are not immune to these effects. Although heart disease usually affects older adults, viral infections can still raise short-term heart risks in healthy individuals.
Dr. Kosuke Kawai emphasized that viral infections can raise the risk for heart complications across all age groups. “Younger individuals often perceive themselves as low-risk, but viral infections can temporarily change that risk profile,” he said. “Even if the overall likelihood remains low, a significant rise in risk following infection can lead to unexpected cardiac events. ”This trend was evident during the COVID-19 pandemic, when otherwise healthy individuals developed myocarditis, pericarditis, and other cardiac complications. In many cases, these issues emerged weeks after the initial infection, underscoring the delayed nature of viral impacts on the heart.
Public health experts now recommend that young adults take infection prevention more seriously, particularly during viral seasons. Vaccination, regular medical checkups, and awareness of warning signs — such as chest discomfort, palpitations, and fatigue after viral illness — can make a critical difference.
Research on Gender and Lifestyle Differences
The relationship between viral infections and heart disease also appears to vary between genders. Studies show that men may be slightly more prone to post-viral cardiovascular complications, likely due to hormonal differences and immune response patterns. However, women are not exempt; some data suggest they may experience longer-lasting inflammatory responses after viral infections.
Lifestyle factors amplify these risks. Smokers, individuals with sedentary lifestyles, or those with high blood pressure or diabetes are more susceptible to post-infectious Viral infections increase heart attack risk cardiovascular events. Viral infections can act as a “trigger” that tips an already vulnerable cardiovascular system toward acute disease.
Dr. Scott Roberts noted that risk is cumulative. “If someone has preexisting hypertension, obesity, or elevated cholesterol, and then they contract a severe viral infection, the stress placed on the heart is exponentially greater,” he said.
The Role of Vaccination in Reducing Cardiovascular Events
Vaccination remains one of the most effective tools for reducing both infection rates and the cardiovascular risks that follow. Flu, shingles, and COVID-19 vaccines help reduce severe illness, hospitalizations, and related heart complications. According to the WHO, influenza vaccination reduces the risk of major adverse cardiovascular events by approximately 36% among high-risk patients. Similarly, COVID-19 vaccination has been linked to fewer cases of myocarditis and blood clots. Vaccinated people face a lower risk of heart attack after viral infections compared to those who are unvaccinated.
Experts emphasize that vaccine hesitancy remains a major barrier to progress. Misinformation, fear, and complacency continue to influence vaccination rates, despite overwhelming evidence of their safety and benefits. Health organizations are therefore focusing on community engagement, education campaigns, and transparent communication to rebuild public trust.
Dr. Kawai said, “Vaccination isn’t just about preventing infection; it’s about protecting your entire cardiovascular system. The ripple effects of preventing severe viral illness go far beyond what most people realize.”
Antiviral Treatments and Post-Infection Care
While vaccines play a preventive role, antiviral medications are crucial for reducing complications once infection occurs. Drugs such as oseltamivir for flu lessen infection severity and protect heart health. Hepatitis C and HIV therapies offer similar protection.
Timely treatment is essential. Delayed diagnosis or failure to complete antiviral regimens can lead to prolonged inflammation, creating ideal conditions for cardiovascular damage. Medical professionals advise cardiac checkups for patients recovering from major viral infections, as viral infections increase heart attack risk. Anyone who experiences breathlessness, irregular heartbeat, or chest pain should seek immediate evaluation.
The WHO and American Heart Association both advocate for integrated healthcare approaches that address infection management and cardiovascular monitoring together. Such strategies are particularly important for elderly patients and those with chronic health conditions.




