Introduction
Pulmonary hypertension is a serious and progressive condition that affects the arteries responsible for transporting blood from the heart to the lungs. Unlike regular high blood pressure, which occurs in the systemic arteries throughout the body, specifically targets the pulmonary arteries. This makes it a unique condition that requires different diagnostic methods, treatment strategies, and long-term care.
Many individuals living with pulmonary hypertension experience symptoms that develop gradually, often mistaking them for ordinary tiredness or effects of aging. Because early signs can be subtle, the condition may go undetected for long periods until symptoms worsen. Understandion is important for early identification, effective management, and improved quality of life.
This article provides a clear and comprehensive explanation of pulmonary hypertension, from how the heart and lungs function together to the long-term effects of elevated pulmonary pressure. It also explores the causes, risk factors, symptoms, diagnostic procedures, treatment options, and lifestyle strategies that can help individuals manage the condition. This guide offers information from introduction to conclusion to support anyone seeking to learn more about
What Is Pulmonary Hypertension?
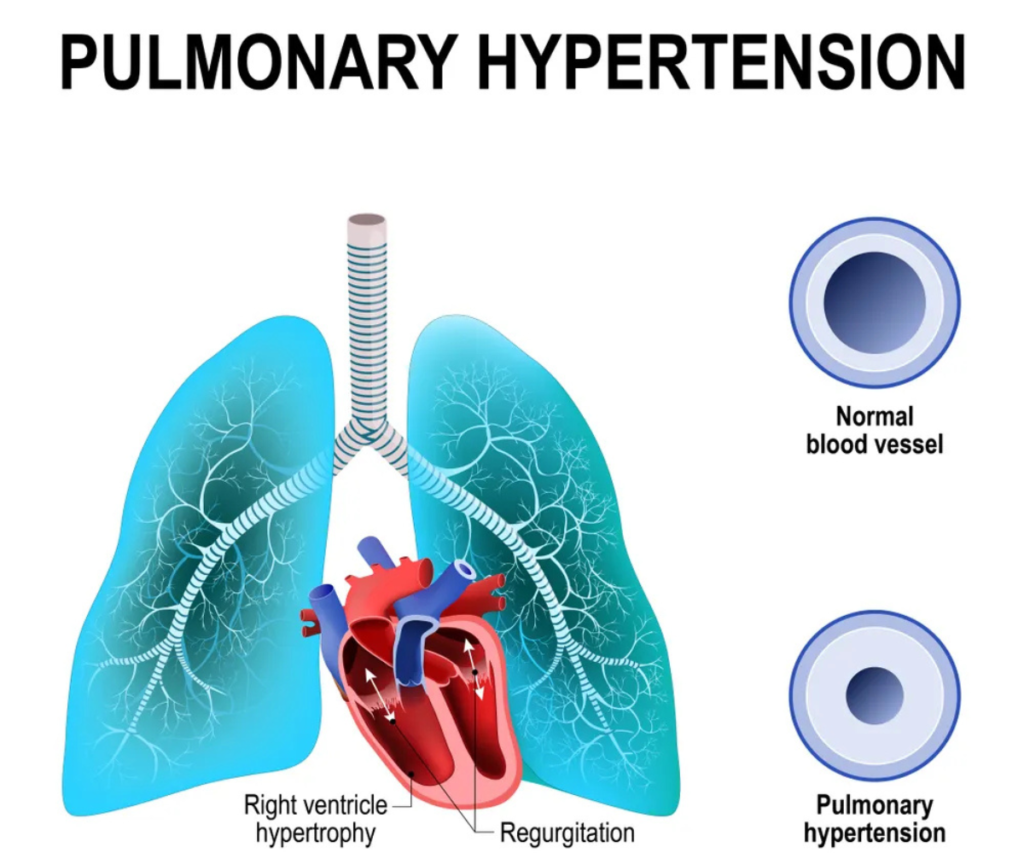
Pulmonary hypertension is a condition in which the pressure inside the pulmonary arteries becomes abnormally high. These arteries carry deoxygenated blood from the right ventricle of the heart to the lungs, where the blood becomes oxygen-rich. Under normal conditions, the pulmonary artery pressure at rest is between 11–20 mm Hg. When the pressure exceeds this range consistently, pulmonary hypertension is present.
It is important to understand that pulmonary hypertension is not the same as traditional high blood pressure affecting the rest of the body. Systemic blood pressure can be measured with a cuff on the arm, but pulmonary hypertension requires specific tests to measure the pressure inside the lung arteries.
One of the most accurate ways to diagnose pulmonary hypertension is through a procedure called right-heart catheterization, which directly measures the pressure inside the pulmonary artery. This procedure is often performed when pulmonary hypertension is suspected but not confirmed through non-invasive tests.
Pulmonary hypertension can develop due to a variety of health conditions, genetic factors, environmental exposures, or unknown causes. Some forms may be mild and manageable with lifestyle changes and medications, while others can be more serious and require long-term treatment.
How Blood Flows Through the Heart and Lungs
To understand pulmonary hypertension clearly, it is important to know how blood circulates through the heart and lungs. The cardiovascular and respiratory systems work together to ensure that every part of the body receives oxygen-rich blood. Pulmonary hypertension.
The Journey of Blood Through the Heart
Blood flow follows a specific path:
- Right Atrium: Blood that has delivered oxygen to the body returns to the right atrium.
- Right Ventricle: From the right atrium, the blood moves into the right ventricle, which pumps it into the pulmonary arteries.
- Pulmonary Arteries: These arteries carry blood to the lungs to receive oxygen.
- Lungs: In the lungs, blood releases carbon dioxide and absorbs oxygen.
- Left Atrium: Oxygen-rich blood returns to the left atrium.
- Left Ventricle: The left ventricle pumps oxygenated blood throughout the body through the aorta.
This cycle continues throughout life, supporting all bodily functions.
How Pulmonary Hypertension Disrupts This Cycle
When pulmonary hypertension develops, the pulmonary arteries become narrowed, thickened, stiff, or blocked. This increases resistance to blood flow, forcing the right ventricle to work harder. Over time, the right ventricle may enlarge or weaken, affecting its ability to pump blood effectively.
If left untreated, this can lead to serious complications including right-sided heart failure.https://www.youtube.com/watch?v=iIzY0XpjgFs
Why Pulmonary Blood Pressure Is Normally Lower
Unlike systemic blood pressure, pulmonary blood pressure is lower because the distance blood travels from the heart to the lungs is short. The lungs are located close to the heart, so less force is needed to push blood through the pulmonary system. Because of this:
- Even small increases in pulmonary artery pressure can have major effects.
- Symptoms of pulmonary hypertension often appear when the heart can no longer manage the increased workload.
- The condition requires careful monitoring and medical evaluation. Pulmonary hypertension.
Long-Term Effects of Pulmonary Hypertension
Over time, pulmonary hypertension can cause significant changes inside the heart and lungs.
1. Narrowed or Stiff Pulmonary Arteries
As the arteries become damaged, they resist blood flow, increasing pressure and reducing oxygen transfer.
2. Enlarged Right Ventricle
The right ventricle works harder to push blood into the lungs, causing it to grow in size. This condition is called right ventricular hypertrophy.
3. Reduced Blood Oxygen Levels
Less oxygen reaches the bloodstream, leading to fatigue, shortness of breath, and reduced stamina.
4. Heart Failure
If the right ventricle becomes too weak to pump effectively, right-sided heart failure may occur.
5. Decreased Quality of Life
Symptoms may limit physical activity, travel, work, and daily routines.
Signs and Symptoms
The symptoms of often begin slowly and worsen over time. At first, individuals may ignore or misinterpret their symptoms as signs of aging, stress, or lack of fitness.
Common symptoms include:
- Shortness of breath, especially during activity
- Fatigue or unusual tiredness
- Rapid or racing heartbeat
- Chest discomfort or pressure
- Pain in the upper right side of the abdomen
- Wheezing or persistent coughing
- Feeling faint or light-headed, particularly during exercise
- Decreased appetite
- Swelling in the ankles, legs, or abdomen
- Episodes of fainting
These symptoms may appear mild at first but tend to become more noticeable as the condition progresses.
Risk Factors

Pulmonary hypertension can affect individuals of various ages, but certain factors increase the likelihood of developing the condition.
Age
The risk increases with age, although can also affect younger individuals.
Environment
Exposure to certain environmental factors, such as asbestos or infections caused by specific parasites, may contribute to the development of pulmonary hypertension.
Family History and Genetics
A family history of blood clots or genetic disorders such as:
- Congenital heart disease
- Down syndrome
- Gaucher disease
may increase the risk of pulmonary hypertension.
Lifestyle Habits
Unhealthy habits can also elevate risk, including:
- Smoking
- Illegal drug use
- Poor physical activity levels
Certain Medications
Some prescription medications used to treat conditions like cancer or depression may increase the risk.
Sex
Women are more likely to develop certain types of compared to men.
Medical Evaluation for Pulmonary Hypertension
Because early symptoms are often mistaken for other conditions, proper medical evaluation is essential for an accurate diagnosis.

Health care professionals typically recommend the following tests:
- Blood tests to check for underlying conditions
- Echocardiogram (echo) to evaluate heart function and pulmonary pressure
- Chest X-ray to identify changes in heart or lung structure
- Electrocardiogram (ECG/EKG) to examine the heart’s electrical activity
- Right-heart catheterization to measure pulmonary artery pressure directly
Additional tests may be necessary to identify the underlying cause.




