Introduction to the Chronic Obstructive Pulmonary Disease Process
The Chronic Obstructive Pulmonary Disease Process (COPD) represents one of the most significant public health challenges in the modern world. It is a long-term, progressive lung condition that causes airflow obstruction, breathing difficulties, and irreversible damage to lung tissues. While often associated with smoking, COPD can also develop due to prolonged exposure to environmental pollutants, occupational hazards, or genetic factors. The disease gradually impairs the body’s ability to exchange oxygen and carbon dioxide efficiently, leading to breathlessness, fatigue, and diminished quality of life.

Globally, COPD ranks among the leading causes of death and disability. Millions of individuals live with the condition, often undiagnosed until the disease has significantly progressed. Despite being preventable and manageable, COPD remains a misunderstood condition. Understanding the Chronic Obstructive Pulmonary Disease Process — from its causes and pathology to its management and prevention — is critical for reducing its global impact.
This comprehensive article explores the intricate mechanisms behind COPD, shedding light on how the disease develops, its effects on lung structure, and the strategies available for early detection, management, and lifestyle modification.
Definition and Overview of COPD
According to the World Health Organization, Chronic Obstructive Pulmonary Disease is a preventable and treatable disease characterized by persistent respiratory symptoms and airflow limitation due to airway and alveolar abnormalities. These changes are usually caused by exposure to harmful particles or gases, most commonly from smoking.
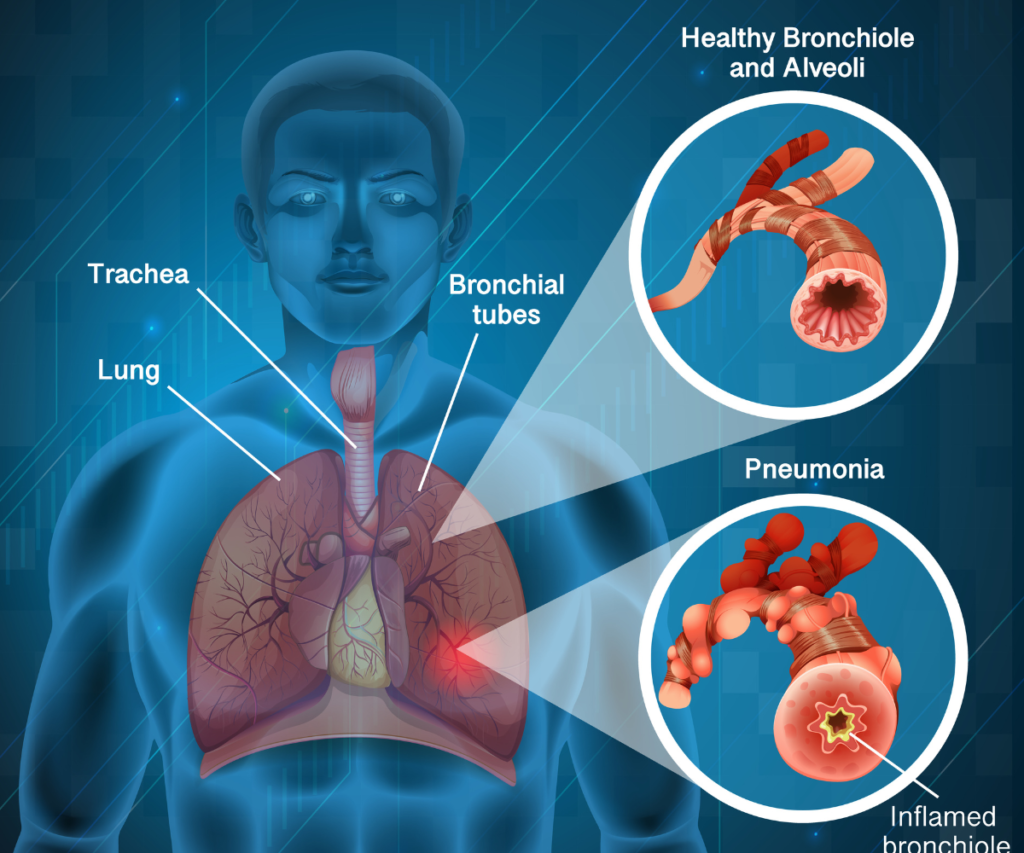
In simpler terms, COPD describes a group of conditions — primarily chronic bronchitis and emphysema — that obstruct airflow in the lungs. This airflow limitation is not completely reversible and tends to worsen over time. As the disease advances, the lungs lose their elasticity, the air sacs (alveoli) are destroyed, and inflammation narrows the airways, making it difficult for air to move in and out.
The Pathophysiological Basis of the Chronic Obstructive Pulmonary Disease Process
The Chronic Obstructive Pulmonary Disease Process begins with inflammation of the airways and lung tissue in response to harmful irritants, such as cigarette smoke, chemical fumes, or dust. This triggers a cascade of biological events:
- Chronic Inflammation – The lining of the airways becomes swollen, and immune cells like macrophages and neutrophils infiltrate lung tissue.
- Mucus Overproduction – The glands in the airways enlarge and produce excessive mucus, clogging small airways.
- Structural Changes – The walls of the airways thicken, lose elasticity, and collapse more easily.
- Alveolar Destruction – The air sacs responsible for gas exchange are damaged, reducing oxygen intake and carbon dioxide removal.
These processes lead to airflow limitation, trapping air inside the lungs, and causing the characteristic shortness of breath seen in COPD patients.
Major Causes and Risk Factors
Smoking and Tobacco Exposure
Smoking is the most significant risk factor for COPD, accounting for up to 90% of cases. Cigarette smoke contains thousands of toxic chemicals that damage the lining of the airways, trigger inflammation, and accelerate tissue destruction. Both active smokers and those exposed to secondhand smoke face a heightened risk.
Environmental and Occupational Pollutants
Individuals exposed to dust, fumes, and chemicals in workplaces such as factories, mining sites, and agricultural settings are at risk of developing COPD. Long-term exposure to biomass fuels used for cooking or heating, especially in poorly ventilated homes, is another major contributor in developing countries.
Genetic Susceptibility
A deficiency in alpha-1 antitrypsin, a protective protein that shields lung tissue from enzyme damage, can make individuals more vulnerable to COPD even if they do not smoke. Genetic factors can also influence the body’s inflammatory response and detoxification ability.
Respiratory Infections and Early-Life Factors

Repeated respiratory infections during childhood or adolescence can lead to poor lung development and increased vulnerability in adulthood. Low birth weight and maternal smoking during pregnancy also correlate with reduced lung function later in life.
Symptoms of Chronic Obstructive Pulmonary Disease
The symptoms of COPD progress gradually and are often mistaken for signs of aging or lack of fitness in the early stages. Common symptoms include:
- Chronic Cough: Persistent and often productive with mucus (sputum).
- Shortness of Breath: Initially during exertion, later even at rest.
- Wheezing: A high-pitched whistling sound during breathing.
- Chest Tightness: Caused by airway constriction and trapped air.
- Fatigue: Due to reduced oxygen delivery to tissues.
- Frequent Respiratory Infections: Inflamed and weakened airways are more prone to infections.
As the disease advances, patients may experience weight loss, muscle wasting, and decreased ability to perform daily activities.
Classification and Stages of COPD
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) classifies COPD based on airflow limitation measured by spirometry:
- Mild (Stage I): Slight airflow limitation with occasional symptoms.
- Moderate (Stage II): Noticeable shortness of breath on exertion.
- Severe (Stage III): Reduced lung function and frequent exacerbations.
- Very Severe (Stage IV): Extreme airflow limitation, chronic respiratory failure, and reduced life expectancy.
Diagnosis of COPD
Early diagnosis is crucial for effective management. The key diagnostic tools include:
Spirometry

Spirometry is the gold standard for diagnosing COPD. It measures the amount of air a person can exhale and how quickly. A FEV₁/FVC ratio (forced expiratory volume in 1 second/forced vital capacity) below 70% confirms airflow limitation.
Chest Imaging
Chest X-rays and CT scans help visualize structural lung changes such as emphysema or airway thickening.
Blood Tests
Blood oxygen levels (arterial blood gas analysis) assess the severity of respiratory failure, while alpha-1 antitrypsin tests identify genetic susceptibility.
Medical History and Physical Examination
A detailed history of smoking, occupational exposure, and symptoms combined with lung auscultation findings helps refine the diagnosis.
Complications and Comorbidities
COPD rarely occurs in isolation. Patients often suffer from co-existing conditions, including:
- Recurrent respiratory infections
- Pulmonary hypertension (high lung blood pressure)
- Osteoporosis
- Diabetes mellitus
- Depression and anxiety
- Sleep disorders
- Lung cancer
These comorbidities complicate management and worsen outcomes, emphasizing the need for comprehensive treatment.
The Progressive Nature of COPD
The Chronic Obstructive Pulmonary Disease Process is progressive. Continued exposure to irritants leads to irreversible damage and lung tissue destruction. The lung’s elastic fibers, responsible for expansion and contraction, deteriorate over time, reducing breathing efficiency.
When inflammation persists, oxygen delivery to organs decreases, forcing the heart to pump harder. This can cause right-sided heart strain (cor pulmonale) — a severe consequence of advanced COPD.https://www.youtube.com/watch?v=W45U1pslKVI
Management and Treatment Options
While COPD has no cure, early intervention and lifestyle modification can slow progression and improve quality of life.
Smoking Cessation
Quitting smoking is the single most effective way to halt disease progression. Behavioral therapy, nicotine replacement, and prescription medications help improve success rates.
Medications
- Bronchodilators: Relax airway muscles (e.g., albuterol, tiotropium).
- Inhaled Corticosteroids: Reduce inflammation.
- Combination Inhalers: Offer dual action for better control.
- Phosphodiesterase-4 inhibitors: Reduce inflammation in severe COPD.
Pulmonary Rehabilitation
A structured exercise and education program helps improve breathing, endurance, and confidence. It includes physical training, nutrition advice, and psychological support.
Oxygen Therapy
Supplemental oxygen is prescribed for those with low blood oxygen levels, helping to relieve symptoms and prevent complications.
Surgery
In select patients, surgical options like lung volume reduction surgery or lung transplantation may be considered.
Lifestyle Modifications and Preventive Care
- Balanced Nutrition: Maintain healthy body weight to support muscle strength.
- Vaccination: Annual flu and pneumococcal vaccines prevent infections.
- Avoid Pollutants: Limit exposure to smoke, dust, and chemicals.
- Regular Exercise: Strengthens respiratory muscles and improves stamina.
- Mental Health Support: Counseling and stress management enhance well-being.
Emerging Research and Future Therapies
Advances in medicine continue to explore new avenues in managing COPD. Current studies focus on:
- Stem Cell Therapy: To regenerate damaged lung tissue.
- Anti-inflammatory Gene Modulation: Targeting cellular pathways involved in chronic inflammation.
- Precision Medicine: Personalizing treatment based on genetic makeup.
- Smart Inhaler Technology: Monitoring patient adherence and optimizing medication use.
These innovations promise a brighter future for those living with COPD.
Preventing COPD: A Public Health Perspective
Prevention is the cornerstone of reducing COPD burden. Public awareness campaigns, stricter air quality regulations, and anti-smoking initiatives play vital roles. Education about early symptoms and routine screening can lead to early intervention, preventing severe disease progression.
Conclusion
The Chronic Obstructive Pulmonary Disease Process represents a complex interaction between environmental exposure, genetic vulnerability, and chronic inflammation. Although irreversible, it is preventable and manageable through early detection, lifestyle modification, and proper medical care. As research advances, understanding and addressing COPD at every stage can empower individuals to breathe easier and live longer, healthier lives.




