Introduction: The Growing Health Crisis
The modern world faces an alarming rise in chronic diseases that often coexist and interact in complex ways. Among the most concerning overlaps are those between heart disease, kidney disease, obesity, and metabolic disorders such as Type 2 diabetes. These conditions are deeply interconnected, influencing each other’s progression and amplifying long-term health risks. The recognition of these overlapping risks of heart and kidney diseases has prompted experts worldwide to redefine how these diseases are identified, prevented, and managed.
Heart and kidney diseases were once viewed as separate medical challenges, each demanding distinct treatment strategies. However, advancing research has shown that these conditions frequently occur together — forming what many experts now refer to as Cardiovascular-Kidney-Metabolic (CKM) Syndrome. This model highlights how the cardiovascular, renal, and metabolic systems work as an integrated network, meaning that damage in one area can trigger deterioration in the others.
Understanding this intricate relationship is vital to improving early detection and implementing preventive care that targets all three systems simultaneously. The aim is not only to treat existing illness but also to halt progression long before it becomes life-threatening.
The Interconnected Web: How the Heart, Kidneys, and Metabolism Are Linked
The human body functions through an extraordinary balance of organs and systems. The heart pumps oxygen-rich blood throughout the body, the kidneys filter waste from that blood, and metabolic processes regulate energy, sugar levels, and fat storage. When one of these systems weakens, the others soon feel the strain.
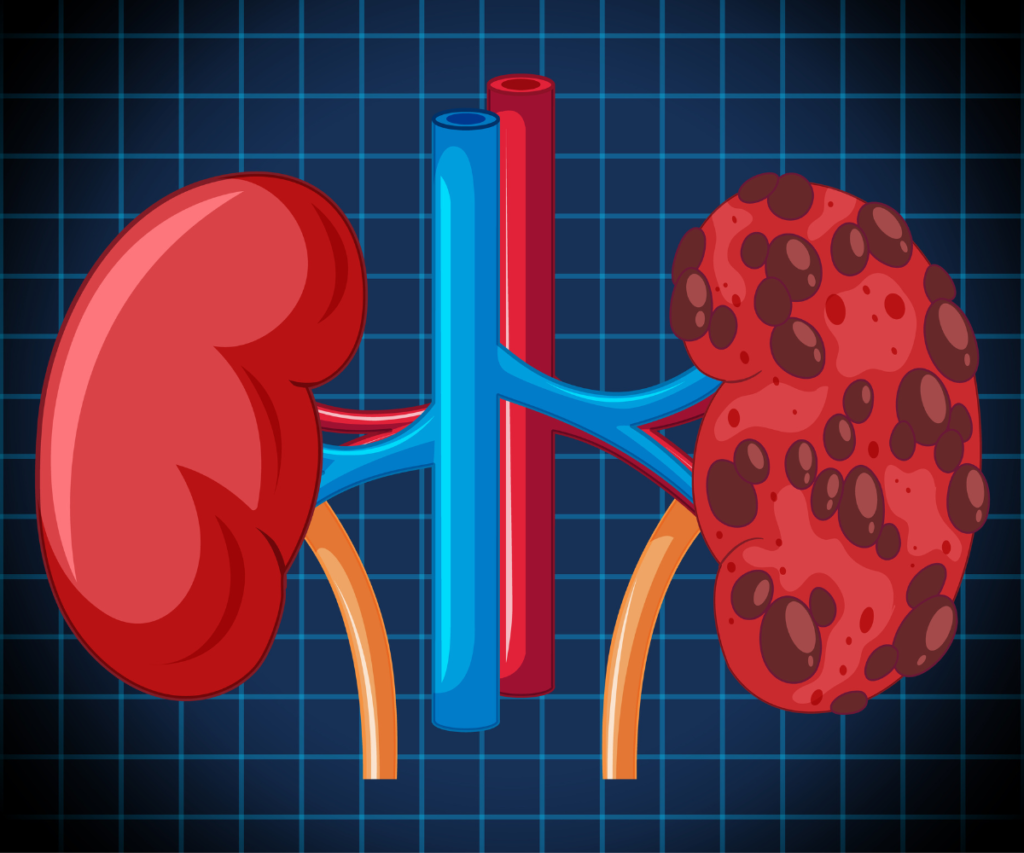
For instance, individuals with Type 2 diabetes often experience high blood sugar levels that damage small blood vessels over time. This damage can impair kidney function, leading to chronic kidney disease (CKD). Simultaneously, high blood sugar levels and inflammation contribute to atherosclerosis—the buildup of fatty deposits in arteries—resulting in increased cardiovascular risk. Likewise, when kidney function declines, toxins accumulate, further straining the heart and circulatory system.
This dynamic interplay shows why tackling each condition in isolation often falls short. Instead, an integrated approach focusing on the overlapping risks of heart and kidney diseases offers more effective outcomes for patients and healthcare systems alike.
The Birth of the CKM Concept
The growing recognition of this complex overlap has given rise to the Cardiovascular-Kidney-Metabolic (CKM) model, a comprehensive framework that identifies patients at risk based on the interrelationship between metabolic dysfunction, kidney impairment, and cardiovascular disease.
Rather than viewing these as three separate conditions, CKM emphasizes a single spectrum of interconnected health risks. It identifies how metabolic issues like obesity, insulin resistance, or high blood pressure can accelerate both heart and kidney damage. This integrated concept encourages early screening, coordinated care, and prevention-focused strategies.
The CKM model also introduces a staged approach to classify patients according to their risk levels and disease progression, helping healthcare professionals tailor interventions more effectively.
The Five Stages of Cardiovascular-Kidney-Metabolic Health
Prevention and Optimal Health
At this stage, an individual has no evident CKM risk factors. The focus is on maintaining good health through balanced nutrition, regular physical activity, adequate sleep, and avoiding tobacco use. Monitoring weight, blood sugar, blood pressure, and cholesterol levels ensures that early warning signs are detected promptly. This stage underscores the importance of primary prevention, emphasizing that the best way to treat disease is to prevent it from developing.
Early Risk Development
Stage 1 marks the beginning of metabolic irregularities. This may include abdominal obesity, prediabetes, or slightly elevated blood pressure. Though symptoms may be subtle, changes in body composition and metabolic efficiency have already begun. Early intervention through lifestyle adjustments—such as losing at least 5% of body weight and improving dietary patterns—can prevent the progression toward more serious disease.
Emerging Disease

At this point, one or more chronic conditions begin to manifest—commonly Type 2 diabetes, hypertension, high triglycerides, or early kidney dysfunction. The body shows signs of systemic strain, as excess glucose and blood pressure begin to damage blood vessels. At this stage, coordinated care becomes crucial. Medications may be introduced to regulate blood pressure, sugar levels, or lipid profiles to prevent the onset of heart failure or kidney failure.
Early Cardiovascular Disease
Individuals in Stage 3 have developed structural or functional heart abnormalities, though they may not yet experience symptoms. Common findings include thickened heart walls, reduced pumping efficiency, or narrowing of arteries. Alongside metabolic and kidney issues, this stage signals significant disease progression. Aggressive treatment—including medication optimization, strict blood sugar management, and lifestyle reinforcement—is required to slow further damage.
Advanced Disease
Stage 4 represents the full expression of Cardiovascular-Kidney-Metabolic Syndrome. At this point, individuals may suffer from heart failure, kidney failure, stroke, or peripheral artery disease. Some may have already experienced a heart attack or developed atrial fibrillation. Treatment becomes more complex and often involves multiple specialists, including cardiologists, nephrologists, and endocrinologists. Despite the advanced stage, lifestyle modifications still play a key role in improving quality of life and preventing further complications.https://www.youtube.com/watch?v=Z9U2_Swya6A
Why the Overlap Matters: Understanding Shared Risk Factors
The overlapping risks of heart and kidney diseases arise from several common factors, many of which are lifestyle-related yet deeply influenced by genetics, environment, and social determinants of health.
1. Obesity and Insulin Resistance
Excess body fat—particularly abdominal fat—releases inflammatory molecules that impair insulin function. This not only increases blood sugar levels but also raises cholesterol and blood pressure, driving both heart and kidney damage.
2. High Blood Pressure
Uncontrolled hypertension forces the heart to work harder and damages delicate kidney tissues. Over time, this leads to thickened arteries and loss of kidney filtration capacity.
3. High Cholesterol
Elevated LDL cholesterol contributes to plaque buildup inside arteries, reducing blood flow to both the heart and kidneys. Reduced circulation deprives organs of oxygen and nutrients, accelerating failure.
4. Type 2 Diabetes
Diabetes remains the single largest driver of CKM-related diseases. Persistent high blood glucose harms small blood vessels, promotes inflammation, and triggers scarring in the kidneys and heart tissue.
5. Sedentary Lifestyle
Physical inactivity slows metabolism, weakens heart function, and contributes to obesity—all of which elevate CKM risk.
6. Poor Diet and Nutrition Insecurity
Diets rich in refined carbohydrates, saturated fats, and excess sodium contribute to obesity, hypertension, and insulin resistance. Limited access to fresh, affordable foods amplifies the problem in low-income areas.
7. Smoking and Alcohol
Nicotine narrows blood vessels and accelerates arterial damage, while alcohol misuse increases triglyceride levels and liver strain, worsening metabolic dysfunction.
The Call for Early Screening and Integrated Care

Experts emphasize that early detection is essential to combating CKM syndrome. Many patients do not realize that subtle metabolic or kidney issues may already be harming their cardiovascular system. Regular screening for blood pressure, cholesterol, fasting glucose, and kidney function markers allows intervention before irreversible damage occurs.
Integrated care models—where cardiologists, nephrologists, and endocrinologists work together—are vital. This multidisciplinary approach ensures that treatment decisions address the full spectrum of disease rather than focusing narrowly on one organ.
Social Determinants of Health: The Hidden Forces Behind CKM
Beyond biology, social and economic factors profoundly shape health outcomes. Individuals with limited access to nutritious food, safe exercise spaces, healthcare services, or education often face higher risks. Addressing these social determinants of health is crucial to reducing the burden of CKM syndrome.
Public health initiatives must therefore expand beyond medical interventions to include community-based education, affordable nutrition programs, and accessible health screenings in schools, workplaces, and local centers.
Updating Risk Prediction Tools
Traditional cardiovascular risk calculators primarily assess short-term risks, such as the likelihood of a heart attack or stroke within ten years. However, such tools often fail to account for kidney function, diabetes control, and long-term metabolic health.
Modernized risk models now aim to include these parameters, extending predictions to 30-year horizons and incorporating early indicators such as albuminuria, glucose variability, and waist-to-hip ratio. Expanding these tools helps healthcare providers identify at-risk individuals much earlier, ideally by age 30, to implement targeted preventive care.
Rethinking Treatment: Beyond Traditional Approaches
The management of overlapping cardiovascular, kidney, and metabolic diseases requires a paradigm shift. Conventional medicine often treats each disease separately—one specialist for diabetes, another for hypertension, and another for kidney function. However, CKM syndrome demands an integrated treatment philosophy.
Lifestyle Interventions
- Emphasis on plant-based, nutrient-dense diets
- Regular aerobic and resistance exercise
- Sleep hygiene and stress management
- Weight reduction as a first-line therapy
Medication and Monitoring
- Use of glucose-lowering agents that also protect the heart and kidneys
- Blood pressure medications that reduce kidney strain
- Cholesterol-lowering drugs to slow atherosclerosis progression
Innovative Therapies
Recent advances in pharmacology have produced drugs that simultaneously benefit all three systems. These dual-purpose medications represent a promising frontier in CKM management, combining glucose regulation with cardiovascular and renal protection.
The Path Forward: Systemic Change in Healthcare
Tackling the overlapping risks of heart and kidney diseases requires systemic reform. Health systems must transition from fragmented care models to integrated structures emphasizing prevention and collaboration.
Education for healthcare professionals should include comprehensive CKM training to ensure early recognition of multi-organ risk. Reimbursement models should incentivize preventive care, lifestyle counseling, and early intervention rather than late-stage treatment.
Governments and public health agencies must also address inequities that contribute to CKM progression—such as food deserts, sedentary urban design, and lack of affordable medical access.
Empowering the Individual: Steps to Protect Long-Term Health
Every individual can take proactive measures to reduce their risk of CKM-related diseases. The following strategies are scientifically supported for long-term prevention:
- Regular Health Screenings – Annual checks for blood sugar, kidney function, and cholesterol
- Balanced Nutrition – Prioritize fruits, vegetables, whole grains, lean proteins, and low sodium
- Weight Management – Maintain a healthy body mass index
- Physical Activity – At least 150 minutes of moderate-intensity activity weekly
- Avoid Smoking and Limit Alcohol
- Manage Stress and Sleep – Chronic stress disrupts hormonal balance, while sleep deprivation worsens insulin resistance
These lifestyle adjustments, though simple, can dramatically reduce disease progression and improve overall vitality.
Conclusion: A Unified Vision for the Future of Health
The recognition of the overlapping risks of heart and kidney diseases marks a pivotal moment in medical understanding. Rather than treating cardiovascular, renal, and metabolic disorders as separate entities, the CKM framework unites them into a single, dynamic continuum of health.
This integrated perspective encourages earlier intervention, more effective prevention, and a patient-centered approach that values long-term well-being over short-term treatment. As healthcare systems evolve, the ultimate goal remains clear — to empower individuals and communities to take control of their health through awareness, education, and collective action.




