Understanding High Blood Pressure
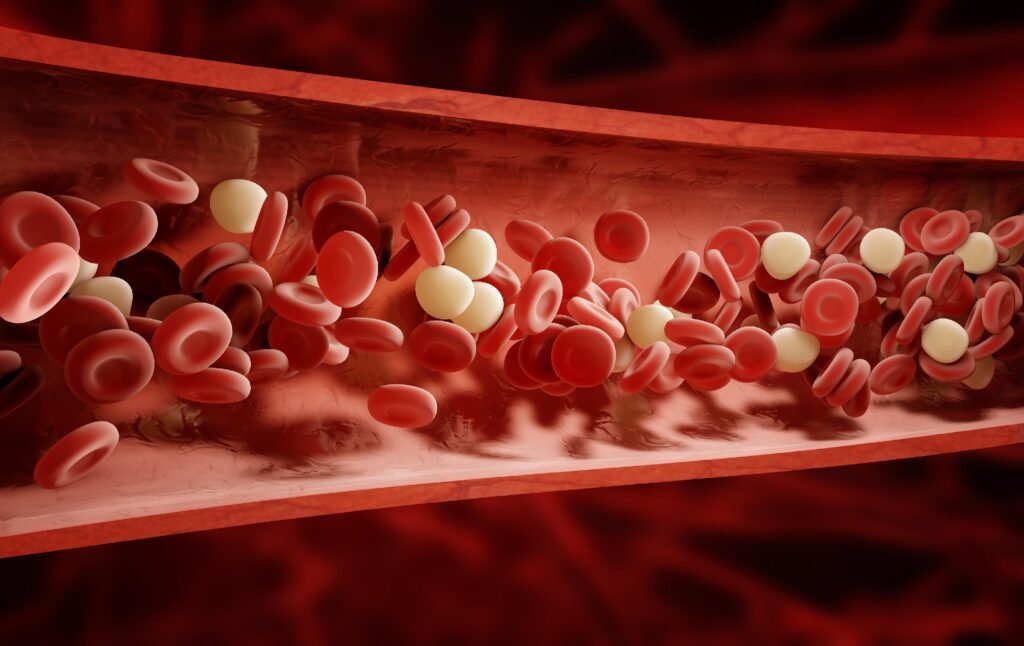
High blood pressure, or hypertension, is a common yet serious condition in which the force of blood against artery walls is consistently too high. This elevated pressure strains the heart and damages blood vessels, increasing the risk of heart attacks, strokes, kidney disease, and cognitive decline. Nearly half of adults have elevated blood pressure, and understanding how to manage it is crucial for long-term health. The latest high blood pressure guidelines emphasize the importance of early detection and intervention, combining lifestyle changes with medical treatment when necessary. Following these recommendations can significantly reduce complications and improve quality of life.
What Counts as High Blood Pressure
Blood pressure is measured in millimeters of mercury, with two readings: systolic pressure, the force of blood as the heart pumps into arteries, and diastolic pressure, the pressure when the heart rests between beats. Normal blood pressure is less than 120/80 mm Hg, while elevated levels fall between 120–129/<80 mm Hg. High blood pressure begins at 130/80 mm Hg, with stage two hypertension defined as 140/90 mm Hg or higher. The updated guidelines encourage healthcare providers to take action at an earlier stage, helping patients adopt healthier habits and, if needed, start medication sooner to prevent long-term damage.

Why Controlling Blood Pressure Matters
High blood pressure is often symptomless, earning it the nickname “silent killer.” Over time, the constant pressure damages arteries and makes the heart work harder, leading to serious complications. Controlling blood pressure reduces the risk of heart attacks, strokes, kidney problems, and vascular damage. It also has a profound impact on brain health, lowering the likelihood of dementia and cognitive decline. Timely monitoring and management are therefore essential for both physical and cognitive well-being.
Lifestyle Changes to Manage Blood Pressure
The new guidelines place strong emphasis on lifestyle changes. Adopting a heart-healthy diet that includes fruits, vegetables, whole grains, lean proteins, and low-fat dairy while limiting salt, sugar, and unhealthy fats can have a major impact. The DASH diet is recommended for reducing blood pressure and supporting overall cardiovascular health. Regular physical activity, such as walking, cycling, swimming, or strength training, strengthens the heart, improves blood circulation, and helps maintain a healthy weight. Weight management is crucial, as even a five percent reduction in body weight can lower blood pressure. Avoiding alcohol is strongly advised, as even moderate drinking can elevate blood pressure and increase cardiovascular risk. Stress management techniques, including meditation, mindfulness, and relaxation exercises, further support healthy blood pressure levels.
When Medication Is Necessary
If lifestyle modifications do not bring blood pressure within target ranges after three to six months, healthcare providers may recommend medication. Various classes of drugs, including diuretics, ACE inhibitors, ARBs, calcium channel blockers, and beta-blockers, are used depending on the patient’s overall health, age, and risk factors. Medication works best alongside continued lifestyle changes and regular monitoring.
Blood Pressure and Pregnancy
High blood pressure during pregnancy can lead to complications such as preeclampsia and long-term hypertension. The guidelines highlight the importance of monitoring blood pressure before and during pregnancy. Maintaining healthy blood pressure levels safeguards both maternal and fetal health and reduces the risk of future cardiovascular problems. https://www.cdc.gov/high-blood-pressure/index.html
Alcohol and Blood Pressure
The new guidelines stress that alcohol can significantly affect blood pressure. Abstinence is ideal, but for those who choose to drink, it is recommended that women limit intake to one drink per day and men to two. Alcohol can worsen blood pressure control and reduce the effectiveness of other interventions. By limiting alcohol, individuals improve cardiovascular health and reduce the risk of related complications.
Protecting Brain Health Through Blood Pressure Control
Managing blood pressure also protects cognitive function. Studies show that consistent control of blood pressure lowers the risk of dementia, memory loss, and other forms of cognitive decline. Both prevention and early treatment of hypertension are crucial for long-term brain health, highlighting the connection between cardiovascular and neurological well-being.
Practical Steps for Maintaining Healthy
Adopting a healthy diet, staying active, monitoring blood pressure regularly, avoiding alcohol, and managing stress are effective ways to maintain optimal blood pressure. Combining these practices with medical supervision ensures early detection of any issues and reduces the risk of severe complications. Lifestyle changes should be gradual, sustainable, and adapted to each individual’s needs and capabilities.
The Importance of Early Action
Starting blood pressure management early can prevent irreversible damage to the heart, kidneys, and brain. The new guidelines encourage both healthcare providers and patients to be proactive, combining lifestyle changes, routine monitoring, and medications when necessary.




