Introduction
Deadly fungal infections are rising across the globe, posing an increasing threat to public health. Traditionally overlooked compared to bacterial and viral diseases, fungal pathogens are now recognized for their ability to cause severe illness, especially among immunocompromised individuals and those with pre-existing respiratory conditions. As global temperatures climb and extreme weather events become more frequent, scientists warn that fungi such as Aspergillus, Candida, and Cryptococcus may spread into new regions, increasing the risk of outbreaks. Understanding the causes, symptoms, and preventive strategies for these infections is essential for individuals, healthcare providers, and policymakers worldwide.
The Global Rise of Deadly Fungal Infections
Recent research highlights that fungal infections kill millions each year, yet reliable data is limited. Environmental factors, including rising temperatures, humidity changes, and extreme weather, are enabling pathogenic fungi to expand their habitats. This expansion increases exposure for populations previously considered low-risk. In particular, Aspergillus fumigatus and Aspergillus flavus are predicted to move into temperate and tropical regions, while resistant strains of Candida auris continue to spread in healthcare facilities, challenging infection control protocols.

High-Risk Populations and Vulnerable Groups
Deadly fungal infections rising disproportionately affect people with weakened immune systems, including cancer patients, organ transplant recipients, and individuals living with HIV/AIDS. Patients recovering from severe respiratory illnesses, such as influenza or COVID-19, are also increasingly vulnerable to opportunistic fungal infections. In addition, older adults and those with chronic lung conditions face higher mortality rates from invasive fungal diseases. Understanding these risk factors is crucial for early detection and intervention.
Impact of Climate Change on Fungal Spread
Climate change is a major driver of the rising prevalence of fungal infections. Warmer temperatures allow fungi to survive in areas previously inhospitable to them, while extreme weather events like floods and droughts can disperse spores over long distances. Researchers have used climate models to predict the spread of Aspergillus species to new regions in North America, Europe, and Asia. These fungi are not only dangerous to human health but also pose risks to agriculture and food security, with some species affecting crops such as maize and peanuts.
Symptoms and Diagnosis of Deadly Fungal Infections
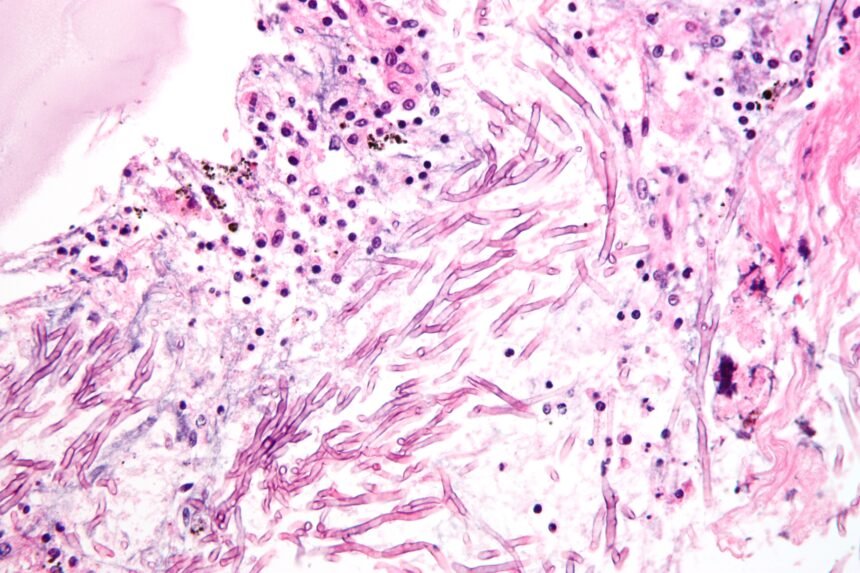
Deadly fungal infections rising present a broad spectrum of symptoms, making diagnosis challenging. Common manifestations include persistent cough, fever, shortness of breath, chest pain, fatigue, and organ-specific effects like vision or hearing impairment in cases of systemic spread. Opportunistic infections such as candidemia and invasive aspergillosis often require laboratory confirmation through blood cultures, imaging, or biopsy. Delays in diagnosis contribute significantly to high mortality rates.
Treatment Challenges and Antifungal Resistance
The rising incidence of fungal infections is compounded by limited treatment options and increasing resistance to antifungal medications. Only four major classes of antifungals—azoles, echinocandins, polyenes, and allylamines—are available, and resistance in strains like Candida auris threatens effective therapy. Long treatment durations and drug side effects further complicate patient adherence. Researchers are exploring new antifungal compounds and combination therapies to address these challenges.
Global Health Implications
Deadly fungal infections rising pose significant challenges for healthcare systems worldwide. Hospitals face the dual burden of treating immunocompromised patients while controlling the spread of resistant strains. In low- and middle-income countries, inadequate diagnostic infrastructure, lack of awareness, and limited access to medications exacerbate the problem. Without proactive measures, fungal infections could become a major global health crisis, especially in regions impacted by climate change. https://www.who.int/news/item/25-10-2022-who-releases-first-ever-list-of-health-threatening-fungi

Prevention Strategies and Public Health Measures
Preventing fungal infections requires a combination of public health interventions, environmental controls, and personal protective measures. Hospitals implement infection control protocols, including isolation of infected patients and strict hygiene measures. Public health agencies advocate for early detection, widespread awareness campaigns, and investment in diagnostic tools. Individuals at high risk are encouraged to practice preventive hygiene, avoid environments with high fungal spore concentrations, and follow medical guidance for immune system support.
Research and Future Directions
Scientific research on fungi is gaining momentum, highlighting the urgent need to understand these pathogens in a changing climate. Ongoing studies focus on fungal genomics, resistance mechanisms, and novel antifungal drug development. Global surveillance programs aim to map fungal prevalence, track emerging strains, and develop predictive models for outbreaks. Increased investment in research and public health infrastructure is critical to mitigate the growing threat of deadly fungal infections.
Conclusion
The rise of deadly fungal infections is a pressing global health concern, amplified by climate change, population vulnerability, and antimicrobial resistance. Awareness, early diagnosis, effective treatment, and preventive strategies are vital to protect at-risk populations and contain outbreaks. As research continues to advance, international collaboration and robust healthcare planning will play pivotal roles in managing this silent but deadly threat.