Introduction: A New Hope for Stroke Survivors
Stroke is a leading cause of long-term disability, leaving many individuals unable to perform everyday tasks independently. Stan Nicholas, a 66-year-old retired musician, experienced this firsthand after a stroke in 2017 left him struggling to move his left side. Traditional physical therapy helped partially, but his recovery plateaued. Enter deep brain stimulation stroke recovery, an innovative treatment that has enabled Nicholas and others to regain mobility, independence, and confidence, highlighting the potential of advanced neuromodulation in stroke rehabilitation.
The Growing Need for Stroke Recovery Solutions
Every year, nearly 795,000 people in the United States suffer a stroke. While emergency care often saves lives, survivors frequently face long-term motor impairments. The current standard of care—physical and occupational therapy—remains essential but is limited in restoring full mobility. Many survivors remain dependent on caregivers for basic activities like cooking, walking, or dressing, creating emotional and financial strain on families. Innovative approaches like deep brain stimulation are emerging to fill this gap, offering hope where traditional therapy falls short.
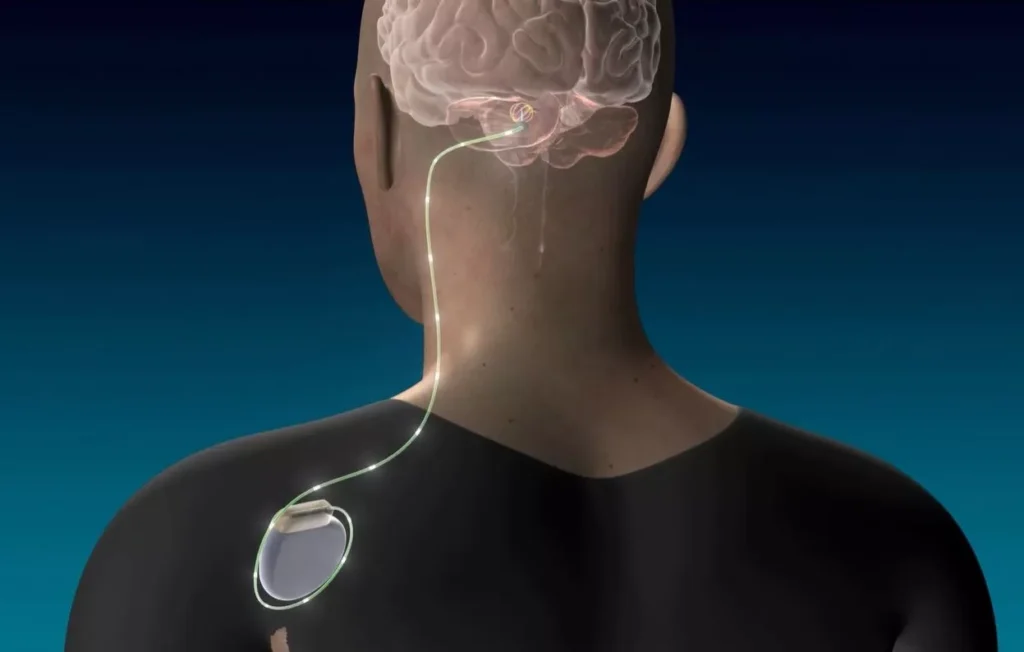
How Deep Brain Stimulation Supports Stroke Recovery
Deep brain stimulation (DBS) involves implanting electrodes into specific regions of the brain that regulate movement and coordination. For stroke survivors, these electrodes target areas connected to motor pathways, stimulating neurons to restore lost function. Unlike conventional rehabilitation, which focuses on muscles and limbs, DBS works at the neurological level, helping the brain “relearn” movement patterns. By integrating with ongoing physical therapy, DBS has the potential to amplify recovery far beyond what therapy alone can achieve.
Nicholas’ Journey: From Disability to Independence
Stan Nicholas, once an avid guitarist performing across Cleveland, experienced a life-altering stroke while preparing dinner in 2017. His left side became severely impaired, leaving him unable to stand or perform basic tasks. Physical therapy improved some function, but his hand remained nearly immobile, and walking was laborious. Feeling desperate but determined, Nicholas volunteered for a pioneering DBS clinical trial.
Doctors implanted electrodes in his cerebellum, connecting them to a device placed under his chest. After several months of gradual adjustments and continued therapy, Nicholas experienced substantial improvements. He regained the ability to grasp objects, walk with stability, and perform daily tasks independently. The combination of DBS and therapy restored not only his physical abilities but also his sense of self and confidence. https://www.nih.gov/news-events/nih-research-matters/stroke-patients-may-benefit-brain-stimulation
The Science Behind Deep Brain Stimulation
The cerebellum, specifically the dentate nucleus, plays a crucial role in coordinating movement and transmitting motor signals to the cerebral cortex. By stimulating this area, DBS creates a ripple effect, enhancing connectivity across neural pathways affected by stroke damage. Originally developed for Parkinson’s disease, DBS demonstrates how adaptable neuromodulation can be for various neurological conditions. Research shows that electrical stimulation can promote neuroplasticity, encouraging the brain to form new connections and compensate for damaged regions.
Physical Therapy and Device Synergy
DBS is most effective when paired with ongoing physical therapy. Nicholas’ therapy included strength training, fine motor exercises, and functional mobility practice. The DBS device amplified the brain’s response to these activities, allowing him to regain movement more efficiently. Experts suggest that combining neuromodulation with conventional rehabilitation may become the gold standard for stroke recovery, particularly for patients whose progress has plateaued.
Clinical Trials and Promising Results
Early trials of DBS for stroke recovery have shown encouraging results. Participants like Nicholas report meaningful improvements in hand and arm function, balance, and overall mobility. Quantitative assessments indicate higher gains than therapy alone, and quality-of-life metrics show enhanced independence and confidence. Researchers continue to study the long-term effects and optimal stimulation protocols, aiming to replicate these outcomes across larger patient populations.
Patient Experiences Highlight New Possibilities
Beyond clinical measures, patient stories underscore the transformative potential of DBS. Survivors report regained autonomy, the ability to engage in hobbies, and renewed social participation. Nicholas, for example, has returned to household tasks, outdoor activities, and even light guitar practice. For many, DBS represents not just a medical intervention but a second chance at a fulfilling life.
Expanding Access to Innovative Stroke Treatments
Despite its promise, access to DBS remains limited. Specialized centers, expert neurosurgeons, and monitoring equipment are concentrated in urban hospitals, posing challenges for rural or underserved populations. Advocates emphasize the need for expanded training, insurance coverage, and outreach programs to ensure more stroke survivors can benefit from this technology. Widespread adoption could transform rehabilitation, offering hope to thousands of individuals who currently face permanent disability.
Long-Term Impact on Quality of Life
For stroke survivors, independence is a key marker of recovery. DBS can restore mobility, enhance self-confidence, and reduce reliance on caregivers. Families, too, experience relief as loved ones regain autonomy. Nicholas’ journey illustrates how the integration of DBS into rehabilitation protocols can profoundly affect everyday life, transforming both clinical outcomes and personal well-being.

The Future of Deep Brain Stimulation in Stroke Recovery
As research progresses, DBS may evolve from an experimental therapy to a standard treatment for post-stroke rehabilitation. Ongoing studies aim to refine electrode placement, stimulation parameters, and patient selection criteria. Innovations such as wireless devices and remote monitoring could further expand access. The combination of neuromodulation, personalized therapy, and patient engagement heralds a new era in stroke recovery, offering renewed hope for millions worldwide.
Conclusion: From Hope to Healing
Deep brain stimulation represents a paradigm shift in stroke recovery. By targeting the brain’s neural networks, DBS provides a path toward restored movement, independence, and quality of life. Patients like Stan Nicholas exemplify the potential of this technology, demonstrating that even after severe stroke-related disability, significant functional recovery is possible. With continued research and broader access, DBS may redefine the future of stroke rehabilitation, offering hope and empowerment to those affected.